- Appendicitis In Pregnancy: 0verview
- Incidence Of Appendicitis During Pregnancy (Is Appendicitis Common During Pregnancy?)
- What Causes Appendicitis In Pregnancy?
- Symptoms Of Appendicitis While Pregnant
- Diagnosis Of Appendicitis During Pregnancy
- Treatment Of Appendicitis During Pregnancy
- Complications Of Appendicitis In Pregnancy
- Recovery From Appendectomy While Pregnant
- FAQs By Patients
- When to Seek Medical Attention
- Conclusion
Appendicitis In Pregnancy: 0verview
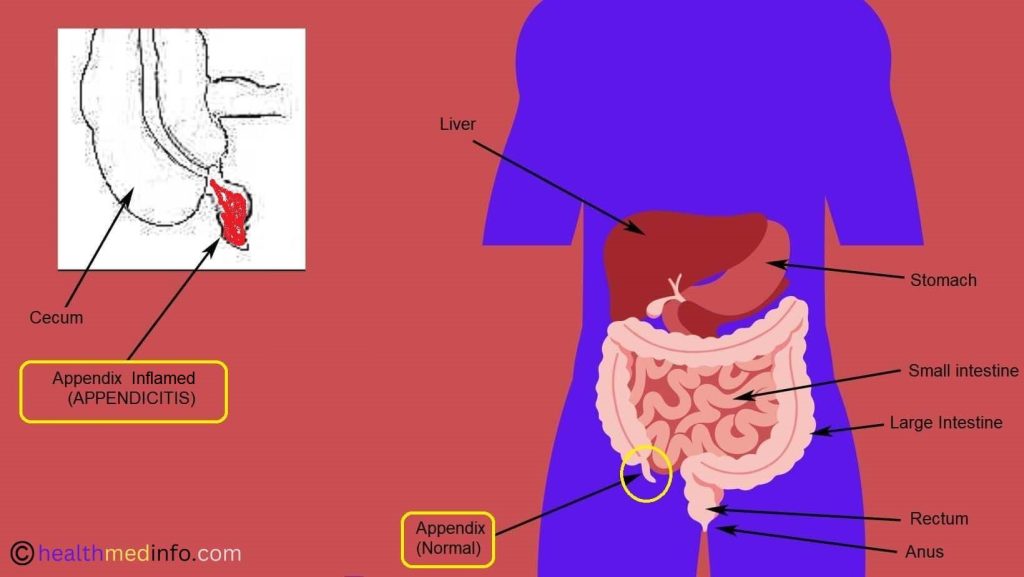
Appendicitis is the medical term that refers to the inflammation of the appendix, a finger-like pouch that is attached to the caecum and projects towards the lower right side of the abdomen. Appendicitis can occur in individuals of any age group, including pregnant women. Developing appendicitis in pregnancy is the most common reason for requiring surgery while pregnant. Pregnant women typically experience appendicitis during the first two trimesters of pregnancy, although it can also occur in the last trimester.
It is very difficult, tricky, and challenging to diagnose acute appendicitis during pregnancy because:
- the classical symptoms of acute appendicitis (such as abdominal pain, nausea, and vomiting) can be very difficult to discriminate from pregnancy-related signs and symptoms.
- Displacement of the appendix by the pregnant uterus leading to confusing physical examination signs.
- The normal increase in white blood cells that occurs during pregnancy can mask the elevated white blood cell count typically seen in appendicitis.
- Radiation exposure from imaging tests, such as a CT scan, is a concern during pregnancy, which further limits the use of imaging for diagnosing appendicitis.
Because of the difficulty in timely and accurate diagnosis of acute appendicitis in pregnancy, pregnant women are more likely to experience perforation of the appendix, adversely affecting the health of the mother and the fetus.
In this article, we will discuss every aspect of appendicitis during pregnancy in detail. Keep on reading!
Incidence Of Appendicitis During Pregnancy (Is Appendicitis Common During Pregnancy?)
The occurrence of appendicitis is relatively rare during pregnancy, with an incidence of 0.05% to 0.07% of pregnancies. However, acute appendicitis is the most common emergency in pregnancy that requires surgical intervention. It is estimated that approximately 1 in 1500 pregnancies is affected by acute appendicitis and requires an appendectomy.
The incidence rates of appendicitis in different trimesters are as follows:
- First trimester: 19% to 36%
- Second trimester: 27% to 60%
- Third trimester: 15% to 33%
Thus, we see that the incidence of appendicitis during pregnancy is higher in the second trimester and decreases in the third trimester, although some studies have shown up to 59% of cases occurring in the third trimester.
What Causes Appendicitis In Pregnancy?
Appendicitis can occur in people of all ages, ranging from children to very old people. It can also strike during pregnancy; however, it is not frequently observed during this time. Appendicitis occurs due to various reasons, and sometimes the exact cause may not be known clearly. Some of the possible causes of appendicitis during pregnancy include, but are not limited to:
- Changes in Hormones: During pregnancy, hormonal changes can affect the digestive system and increase the risk of constipation, which can lead to the blockage of the appendix and inflammation.
- Pressure from the Uterus: As the uterus expands during pregnancy, it can put pressure on the appendix and cause it to become obstructed and inflamed.
- Blockage of the appendix due to hardening of stool because of parasites, constipation, etc.
- Blockage of the appendix due to cancer or accidental ingestion of foreign bodies (such as pins, stones, bullets, etc.)
- Formation of a stone in the appendix (appendicolith) due to the calcification of fecal materials
- Inflammatory bowel diseases.
- Infections in the digestive tract or elsewhere in the body, causing enlargement of tissue in the wall of the appendix.
Whenever the lumen of the appendix gets blocked by any of the above-mentioned reasons, bacteria start proliferating in the lumen of the appendix, leading to infection and inflammation of the appendix.
Some studies suggest the role of genetic factors in contracting appendicitis. It was found that a positive family history increases the risk of developing acute appendicitis almost three times.
Symptoms Of Appendicitis While Pregnant
Pregnant women are less likely to present with the “classic symptoms” of appendicitis due to changes in appendix location caused by the enlargement of the uterus and the high prevalence of abdominal or gastrointestinal discomfort. Hence, an ultrasound scan is recommended to confirm the diagnosis of appendicitis in all suspected pregnant women. Perforation of the appendix occurs more often in pregnant individuals, especially in the third trimester, possibly due to the following reasons:
- Challenges in diagnosing acute appendicitis in pregnancy
- Delayed diagnosis and treatment in pregnant individuals
- Reluctance to operate on pregnant individuals
Signs and symptoms of appendicitis in pregnancy may include:
- Right Lower Quadrant (RLQ) abdominal pain
- Right lower quadrant (RLQ) tenderness
- Nausea
- Vomiting
- Diarrhea
- Anorexia (lack of appetite)
- Uterine contraction
- Dysuria (painful urination)
- Rectal and vaginal tenderness, especially in the first trimester
Fever and tachycardia may not be present in appendicitis during pregnancy. Only a few pregnant individuals with appendicitis are going to have a very high fever (only 20% of patients will have a temperature >100°F), and the reason for this is not clear.
Additionally, if a pregnant woman is in her third trimester, she may experience pain or tenderness in the Right Upper Quadrant (RUQ) instead of the Right lower quadrant (RLQ) just below the lowest rib on the right side. This is because as the fetus grows in the womb, the appendix goes higher up in the abdomen.
If you experience any symptoms of appendicitis during pregnancy, seek medical attention right away.
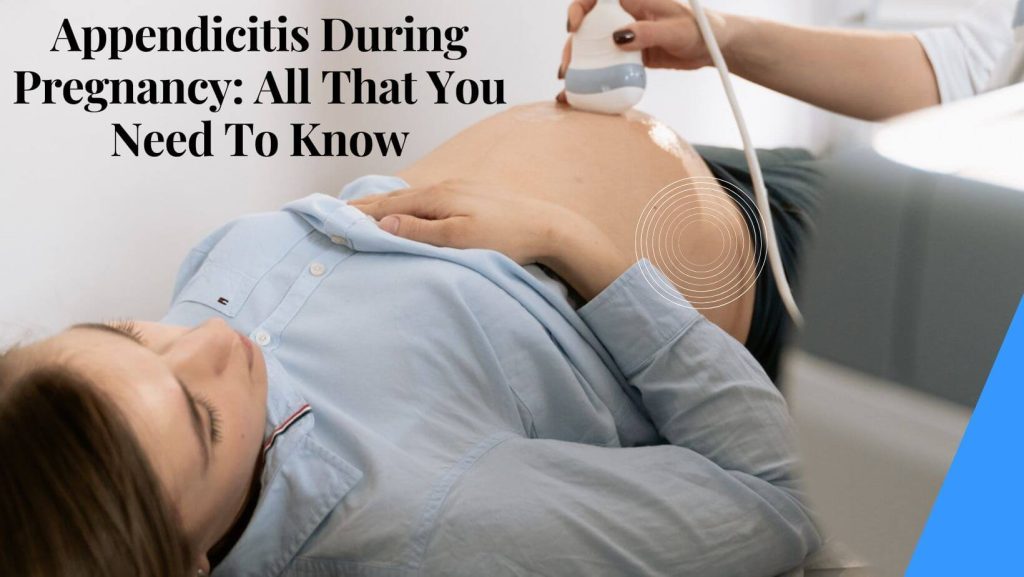
Diagnosis Of Appendicitis During Pregnancy
Accurately identifying acute appendicitis in pregnancy can be a diagnostic challenge as symptoms of appendicitis are similar to pregnancy symptoms. Therefore, several methods/tests/procedures are adopted to confirm the diagnosis. Usually, the diagnosis of appendicitis during pregnancy typically involves a combination of physical examination, medical history, laboratory tests, and diagnostic imaging tests.
Here are some of the methods, tests, and procedures that are used for diagnosing appendicitis during pregnancy:
History taking: In the very first step medical history of the patient is obtained to know other possible causes of similar signs and symptoms.
Physical examination: The doctor will perform a physical examination to check for signs of inflammation and tenderness in the abdomen, particularly in the lower right side where the appendix is located. They will press around the abdomen to identify painful areas, and they will also tap and test for rebound tenderness, i.e., pain after the release of pressure of hand. They will also check for fever, nausea, vomiting, and other symptoms.
Blood tests: Complete blood count (CBC) is done to find out the white cells count. White blood cell counts usually increase with appendicitis. But this test is less helpful in pregnant individuals than in other patients. Because the white blood cell counts are already high in pregnancy. So an elevated white blood cell counts does not necessarily indicate appendicitis in pregnancy.
Urine Test: A urine test is also ordered since appendicitis can result in urinary tract infections (UTIs)
Imaging Tests: Routine imaging is recommended in all pregnant women with suspected appendicitis to obtain accuracy in diagnosis and to eliminate the risk of negative appendectomy (surgical removal of appendix).
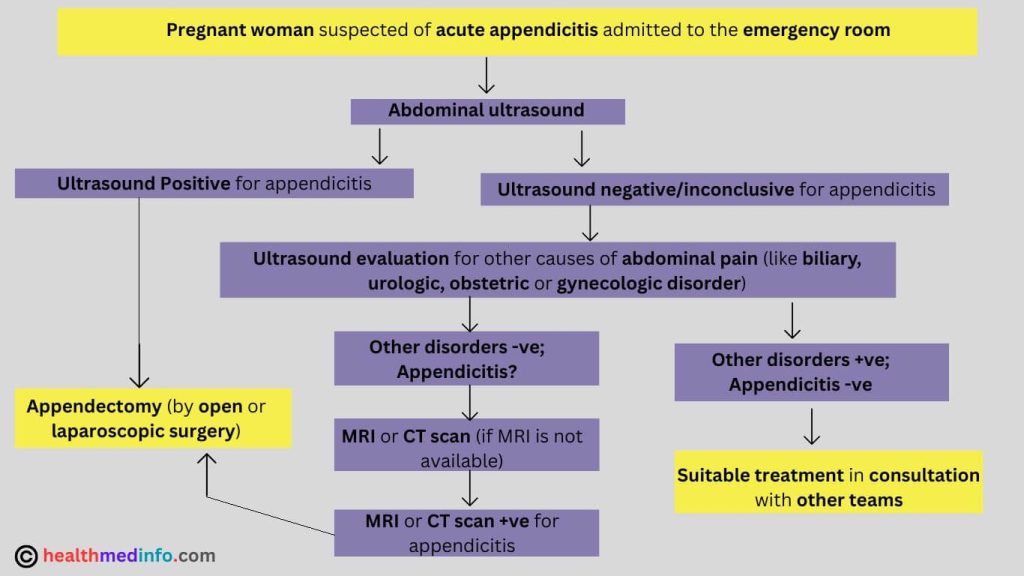
When a pregnant woman arrives in the emergency room of a hospital with symptoms indicative of appendicitis then an abdominal ultrasound is recommended as the first line of diagnosis because:
- It is pregnancy safe and easily available.
- It also provides information on fetal well-being and obstetric causes of abdominal pain.
If the ultrasound results are inconclusive then magnetic resonance imaging (MRI) without gadolinium contrast is used for confirmation or exclusion of appendicitis during pregnancy. It also carries no risk of radiation and it provides good soft-tissue resolution. According to some authorities when ultrasound is inconclusive and MRI is not available, then the use of CT scan might be allowed. According to some researches, the use of CT scan reduces the rate of negative appendectomy greatly in comparison to clinical assessment alone or when combined with ultrasound. But doctors recommend a limited CT scan below the threshold to help reduce the risk of ionizing radiations to the baby and fetal malformations.
Differential Diagnosis Of Appendicitis In Pregnancy:
There are many obstetrical and gynecological conditions and nonobstetrical and nongynecological conditions that share similar signs and symptoms with acute appendicitis (like pain in the lower right quadrant of the abdomen).
Differentials to be considered In pregnant patients for appendicitis are given below.
| Obstetrical/gynecological conditions that mimic appendicitis include: | Nonobstetrical/nongynecological conditions that mimic appendicitis include: |
| Tubo-ovarian abscess, pelvic inflammatory disease (PID), threatened abortion, salpingitis, ruptured ovarian cyst, ovarian torsion, fallopian tube torsion, ectopic pregnancy , round ligament syndrome, hemorrhagic ovarian cyst, preeclampsia, placental abruption, HELLP (hemolysis, elevated liver function tests, low platelets) syndrome, and uterine rupture. | Cecal diverticulitis, Meckel’s diverticulitis, acute ileitis, inflammatory bowel disease (Crohn and ulcerative colitis), renal colic, and urinary tract infections, gastroenteritis, pyleonephritis, cholecystitis, cholelithiasis, nephrolithiasis, pancreatitis, hernia, bowel obstruction, carcinoma of the large bowel, mesenteric adenitis, rectus hematoma, right-lower-lobe pneumonia, pulmonary embolism, and sickle cell disease. |
As the symptoms of appendicitis can be very similar to those of other conditions, it is important for pregnant women experiencing these symptoms to seek medical attention to get an accurate diagnosis and appropriate treatment.
The doctors review the medical history and conduct several examinations on the pregnant patient with suspected acute appendicitis, in order to reach an accurate diagnosis.
Treatment Of Appendicitis During Pregnancy
Appendicitis during pregnancy is treated by two methods, depending on the severity of the condition, the stage of pregnancy, and the overall health of the mother and baby.
These methods are:
- Antibiotics: If the inflammation is mild, and there is no risk of perforation of appendix, then antibiotics may be recommended for treatment. This may be helpful in reducing the infection and the related symptoms. The antibiotics can be given intravenously for faster and better action.
- Appendectomy: After appendicitis is confirmed during pregnancy, appendectomy (=surgical removal of the appendix) is indicated in most cases. Appendectomy is usually considered as the curative treatment of acute appendicitis in pregnant women. The risk of appendix perforation increases after the first 24 hours of the start of the symptoms. That’s why early diagnosis and surgical intervention are of great importance to preserve the patient’s health and pregnancy. Perioperative antibiotic treatment is provided against gram-positive and gram-negative bacteria (usually with a second-generation cephalosporin) and anaerobic bacteria (with clindamycin and metronidazole).
Appendectomy during pregnancy is performed in one of the two ways:
Open surgery: during which the inflamed appendix is removed through a single large incision
Laparoscopic surgery: during which the inflamed appendix is removed through a few small cuts on the abdomen.
Appendectomy by laparoscopic surgery (also known as band-aid surgery) is preferred over open surgery because in this method the cuts are smaller, pain is less, blood loss is less, recovery is faster, and chances of complications after operation are reduced.
However, the selection of the method of appendectomy depends on several factors like the gestational age, medical history and clinical status of the pregnant woman and her baby, and the surgeon’s experience.
If the patient is in the first or second trimester, then she is likely to have a laparoscopic surgery. Whereas if the patient is in the third trimester, then she is likely to have an open surgery as the size of the gravid uterus makes laparoscopy difficult.
New Researches Find:
Pregnant women who undergo an appendectomy, whether through laparoscopic or open surgery, may experience preterm contractions, but only a small fraction of them (about 10%) will give birth prematurely. However, the risk of early delivery increases as the pregnancy advances, with 8% of cases occurring before 24 weeks of gestation, 13% between 24 and 28 weeks, and 35% between 29 and 36 weeks.
While surgery is the typical course of action for uncomplicated appendicitis, it is possible to treat it without surgical intervention. Recent research has investigated the feasibility of utilizing antibiotics as a conservative, non-surgical approach to treat uncomplicated appendicitis. Despite this, the method is not widely accepted and may increase the chances of appendicitis recurring.
Therefore, patients and their doctors should have a conversation about alternative treatment options and the associated risks, including those related to the pregnancy.
Complications Of Appendicitis In Pregnancy
Though appendicitis during pregnancy is relatively rare but it is a potentially serious condition that requires immediate medical attention and medical interventions. The complications of appendicitis during pregnancy can be more severe than in non-pregnant individuals due to the anatomical and physiological changes that occur during pregnancy. Some of the possible complications of untreated appendicitis during pregnancy include:
- Peritonitis: Peritonitis is a serious complication of appendicitis that occurs when the appendix ruptures resulting in leakage of the infectious content in the abdominal cavity, leading to the inflammation and infection of the peritoneum (abdominal lining). In pregnant women, peritonitis can lead to sepsis, preterm labor, and fetal distress.
- Preterm labor: Appendicitis during pregnancy can cause preterm labor, which is the onset of labor before the 37th week of gestation. Preterm labor can lead to a range of complications, including low birth weight, respiratory distress syndrome, and developmental delays.
- Fetal distress: Fetal distress is a condition in which the fetus does not receive enough oxygen or nutrients, leading to abnormal fetal heart rate patterns. This condition can occur due to the inflammation and infection caused by appendicitis, and can lead to fetal brain damage, cerebral palsy, and stillbirth.
- Maternal complications: Appendicitis during pregnancy can cause a range of maternal complications, including sepsis, wound infections, and abscess formation. In severe cases, appendicitis can lead to maternal death.
- Miscarriage: In rare cases, appendicitis during pregnancy can lead to miscarriage (fetal loss), particularly if the appendix ruptures and causes widespread infection and inflammation due to delay in diagnosis and treatment of appendicitis.
The surgical procedure (appendectomy) itself can lead to a range of complications, such as infections (such as postoperative peritoneal abscess), bleeding, and injury to neighboring structures.
Pregnant women with appendicitis have a greater likelihood of morbidity and perforation, compared to non-pregnant women. During appendicitis in pregnancy, the rate of perforation of appendix can be as high as 55%, which can increase the risk of miscarriage or preterm delivery if not treated promptly. Delay in diagnosis and treatment can also pose a life-threatening risk to the mother. Unruptured appendicitis can result in a maternal mortality risk of up to 2% and a fetal loss risk of 1.5-9%, with an increased risk if there is perforation. Appendicitis complications, such as appendix rupture, are more common during the third trimester of pregnancy.
Therefore, it is important to seek medical attention immediately if you experience symptoms of appendicitis during pregnancy, such as abdominal pain, fever, nausea, vomiting, and loss of appetite. Early diagnosis and treatment can help to prevent these complications and ensure a safe delivery and good health for both the mother and the baby.
Recovery From Appendectomy While Pregnant
Recovering from appendix surgery (appendectomy) while pregnant depends on various factors, such as the method of surgery, the stage of pregnancy, the overall health of the mother and baby, and any possible complications that may arise during or after the surgery. Open surgery typically requires a longer hospital stay and recovery time compared to laparoscopic surgery. Generally, after an appendectomy, a pregnant woman may need to stay in the hospital for a few days for observation, pain management, and to manage any postoperative complications.
The recovery time for pregnant women may also be longer than non-pregnant women, and it may take a few weeks for them to fully recover and return to normal activities. However, this can differ depending on the patient’s individual circumstances. During this period, they may need to take pain medication, avoid strenuous activity, and follow a specific diet as advised by their doctor.
It is crucial for pregnant women to follow their doctor’s instructions carefully and attend all follow-up appointments to ensure a smooth recovery.
Frequently Asked Questions By Patients:
-
What Happens If Your Appendix Bursts While Pregnant?
If the appendix ruptures or bursts during pregnancy, it can lead to serious complications such as peritonitis, abscess formation, and sepsis. These complications can be life-threatening for both the mother and the developing fetus.
Peritonitis is a condition where the lining of the abdominal cavity (peritoneum) becomes inflamed due to the spillage of infectious material from the burst appendix into the abdominal cavity. It can cause symptoms like fever, severe abdominal pain and tenderness, nausea, vomiting, diarrhea, and shock. Peritonitis requires immediate medical attention and treatment with antibiotics.
Abscess formation is another potential complication of a ruptured appendix during pregnancy. An abscess is a collection of pus that can develop in the abdomen due to infection. It can cause symptoms like fever, chills, abdominal pain and swelling, and nausea. Treatment may require surgical drainage of the abscess and extended antibiotic treatment.Sepsis is a serious and life-threatening condition that can occur when the body’s immune response to an infection becomes overactive, causing widespread inflammation throughout the body. Symptoms of sepsis include fever, rapid heartbeat, rapid breathing, confusion, and low blood pressure. Sepsis requires prompt medical attention and treatment with antibiotics and intravenous fluids.
A burst appendix can also increase the risk of premature labor and delivery, fetal distress, and stillbirth. The baby may require close monitoring and may need to be delivered early to prevent further complications.
The standard treatment of the burst appendix is the appendectomy (surgical removal of appendix). In most cases, a ruptured appendix during pregnancy requires an emergency surgery to remove the appendix and prevent further complications. The timing and type of surgery will depend on the severity of the infection, the gestational age of the fetus, and other factors. It is essential to seek medical attention right away if you suspect you have appendicitis while pregnant. -
Does Appendix Removal Affect Pregnancy?
In general, having an appendectomy (removal of the appendix) should not affect a woman’s ability to become pregnant in the future. The surgery itself does not involve the reproductive organs, so there is no direct impact on fertility. However, there are some factors that could affect a woman’s fertility after an appendectomy.
One potential issue is scarring or adhesions that may form as a result of the surgery. Adhesions are bands of scar tissue that can form between organs and tissues, and they can sometimes cause problems with fertility. For example, adhesions may block the fallopian tubes or interfere with the normal functioning of the ovaries or uterus. This may have the risk of ectopic pregnancy in the future, however, the risk is generally low. -
Is It Safe To Have Appendix Surgery While Pregnant? (Can A Pregnant Woman Have Her Appendix Removed?)
In general, appendectomy is considered safe for pregnant women who require it. However, the decision to perform the surgery depends on several factors, including the severity of the appendicitis, the stage of pregnancy, and the risks and benefits to both the mother and the fetus. Surgery during the first and second trimesters is generally considered safer than during the third trimester, as the risk of preterm labor and delivery is higher in the third trimester. Additionally, surgery during pregnancy may require modifications to the anesthesia and surgical techniques used to ensure the safety of both the mother and the fetus. It is important to discuss the risks and benefits of surgery with your healthcare provider if you are pregnant and have appendicitis. Generally, a laparoscopic appendix surgery during pregnancy is considered safe for both the mother and the fetus, regardless of the stage of pregnancy. Additionally, the incidence of post-operative complications associated with this procedure is low. However, laparoscopic appendectomy may be associated with a significantly higher rate of fetal loss compared with open appendicectomy.
-
What Happens If You Get Appendicitis While Pregnant?
Appendicitis during pregnancy is associated with an increased risk of serious complications, morbidity, and perforation compared to the general population. Because of the challenges in diagnosing appendicitis in pregnant women, perforation rates are higher, adversely affecting both mother and fetus. Furthermore, if not detected and treated promptly it may cause preterm birth and fetal loss. Generally, quick surgical intervention is the established treatment option in pregnant women with acute appendicitis.
-
Can Appendicitis Cause A Miscarriage?
Untreated or delayed treatment of appendicitis during pregnancy can increase the risk of abortion (miscarriage) or preterm labor. This is because the inflammation and infection in the appendix can trigger a response from the body’s immune system, which may also affect the uterus and cause contractions. Additionally, if the appendix ruptures, it can release bacteria and toxins into the bloodstream, which can also harm the developing fetus and increase the risk of pregnancy loss. However, if the appendicitis is diagnosed and treated promptly, the risk of abortion or preterm labor can be minimized.
When To Seek Medical Attention
It is important to seek medical attention if you experience any symptoms of appendicitis during pregnancy. Prompt diagnosis and treatment can help prevent complications and improve outcomes. If you experience severe abdominal pain or any other symptoms of appendicitis, contact your healthcare provider immediately.
Conclusion
In conclusion, appendicitis in pregnancy is a serious medical condition that requires prompt attention and treatment. Pregnant women may get appendicitis, and it is important to be aware of the symptoms. If you experience any symptoms of appendicitis during pregnancy, seek medical attention right away.
References:
- Aptilon Duque G, Mohney S. Appendicitis in Pregnancy. [Updated 2022 Aug 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK551642 [Accessed on March, 2023]
- Ibiebele I, Schnitzler M, Nippita T, Ford JB. Appendicectomy during pregnancy and the risk of preterm birth: A population data linkage study. Aust N Z J Obstet Gynaecol. 2019;59(1):45-53. doi:10.1111/ajo.12807 [Accessed on March, 2023]
- Tamir, I L et al. “Acute appendicitis in the pregnant patient.” American journal of surgery vol. 160,6 (1990): 571-5; discussion 575-6. doi:10.1016/s0002-9610(05)80748-2 [Accessed on March, 2023]
Dr. Jasmine Roy, MBBS, MS
Ostetrician & Gynecologist
 Dr. Jasmine Roy is an esteemed doctor and researcher practicing Obstetrics & Gynecology in Mumbai, the Financial Capital of India. She has published over 50 publications in her areas of expertise, which includes treatment of female sexual problems, caesarean delivery procedure, treatment of pregnancy problems, normal delivery process and breastfeeding. READ MORE…
Dr. Jasmine Roy is an esteemed doctor and researcher practicing Obstetrics & Gynecology in Mumbai, the Financial Capital of India. She has published over 50 publications in her areas of expertise, which includes treatment of female sexual problems, caesarean delivery procedure, treatment of pregnancy problems, normal delivery process and breastfeeding. READ MORE…
Dr. Jennifer Jones, MBBS, MS
Ostetrician & Gynecologist
 Dr. Jennifer Jones is a highly experienced obstetrician and gynecologist, with over 16 years of practice in the field. She has worked in various prestigious hospitals across the United States and India, and currently runs her own private clinic in New Delhi, India. Dr. Jones is widely recognized for her expertise in medically assisted reproduction, hysteroscopy and laparoscopy, cesarean delivery, menstrual-related issues, and hormonal disorders. READ MORE…
Dr. Jennifer Jones is a highly experienced obstetrician and gynecologist, with over 16 years of practice in the field. She has worked in various prestigious hospitals across the United States and India, and currently runs her own private clinic in New Delhi, India. Dr. Jones is widely recognized for her expertise in medically assisted reproduction, hysteroscopy and laparoscopy, cesarean delivery, menstrual-related issues, and hormonal disorders. READ MORE…